If there’s one thing synonymous with this time of year, it’s tax season. And for hospitals, that means it’s time to evaluate if you’re inadvertently making your hospitalists pay the “discharge tax.”
What is the discharge tax?
Most hospital medicine programs aim to evenly balance hospitalists’ workloads – and the simplest way to do that is to make sure that each hospitalist sees the same number of patients. If there are three hospitalists and 45 patients that need to be seen that day, then each hospitalist should get 15.
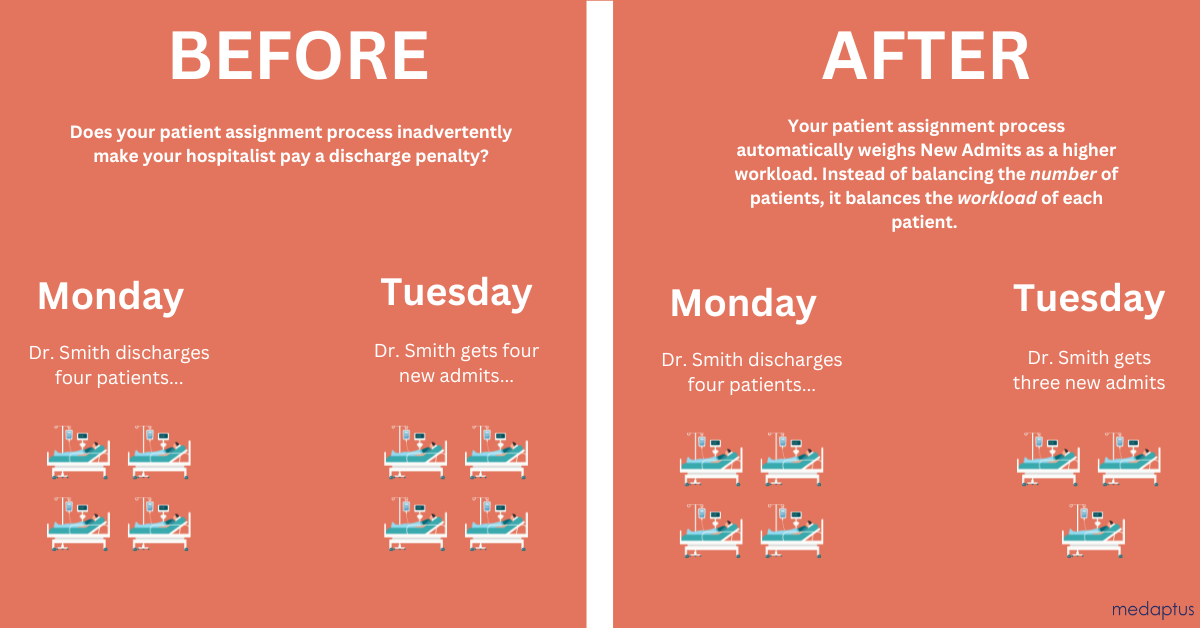
The problem with that (besides for the fact that it doesn’t take into account the complexities of patients, and how some patients – such as new admits – are more work than others), is that when Dr. Smith discharges eight patients today, that means she automatically gets hit with the discharge tax tomorrow – she gets eight new patients. If you discharge a lot of patients today, you get a lot of new patients tomorrow to bring your workload back up.
The downside to this? Well, as a hospitalist myself, we know that this leads to heavier workloads and doesn’t encourage hospitalists to safely discharge as soon as possible.
Why is discharging important for hospital leadership?
Missed revenue
If you go back 40 years when everything was fee for service, hospitals got paid per day, however long the patient stayed. But that’s not how it works today. Now, the patient’s diagnostic related group (DRG) based on what the hospitalist documents, determines how much you can collect per patient. For example, perhaps insurance pays $6000 for pneumonia patients, whether they stay two days or 10.
There’s a multi-pronged approach to keep length of stay down and get patients out of the hospital if they can be safely discharged. That leads to fewer expenses, opens up more beds to start seeing new patients and start collecting revenue on them.
Bed shortages and capacity
In addition to the revenue argument, many hospitals today are running at capacity or over capacity. More than 80% of hospital beds are in use nationwide, according to a CNN report. The ERs are not designed for longitudinal management of patients. It fills up the ED beds which means the ED can’t cycle emergency patients through. And it becomes a real problem when you get really full – now there’s no beds for patients to come out of the OR, and you have to cancel surgeries because there are not enough beds.
Discharging in a timely fashion helps improve throughput in the ED and reduces the risk of patients developing complications from being in the hospital for the long-term.
Analyzing your hospitalists’ discharge rates
If safely discharging patients can help you improve throughput, improve patient care, and free up space for new and more emergent patients, then what prevents hospitalists from discharging their patients? What if you could drill down into your discharge rates and length of stay reports, and understand the trends by hospitalist, by department, or even by season? What if you knew that hospitalist A has an average LOS of six days and hospitalist B has an average LOS of eight days, no matter the patient’s condition. This type of information becomes critical for staffing – when you make the schedule, you can take into account the expected number of patients that will actually be seen and actually discharged. You could predict capacity and the number of available beds, simply by knowing which hospitalist is on call.
For example, in our patient assignment software, Assign, we help our customers understand these trends with the discharge efficiency report – what is the average length of stay per provider per discharge. Hospitals can drill down and understand hospitalists’ personal length of stay. And imagine being able to take into account other factors like seasonality (flu season might increase LOS), or departmental variations.
We know discharging helps patients and hospitals – but we’re punishing hospitalists who do it.
We know that safely discharging patients who are ready to go home on time is good for the patient and good for the hospital – but it doesn’t always mean it’s good for the hospitalist.
Because when a hospitalist discharges five patients today, they are “punished” with the discharge tax and assigned the exact same number of new patients tomorrow. This doesn’t encourage hospitalists to safely discharge on time, since they know they’re getting a heavier workload tomorrow with a crop of new patients.

The alternative?
Using patient assignment software like Assign, we can help you evenly balance patients taking into account a variety of factors – so your hospitalists are not just assigned the same number of patients, but instead the same workload. A new patient could be weighted as 1.2 patients while an ICU downgrade may be 1.3. You can weigh patients that are not new to the hospital but “new to the provider” a little more heavily – so if a hospitalist never saw that patient before, maybe it’s worth 1.3 than a regular patient.
Now, when a hospitalist discharges five patients today, they don’t automatically receive five new patients tomorrow. They receive the equivalent workload – which may actually be fewer patients.
This keeps hospitalists’ workloads in check and reduces the burden of the discharge tax.
In the end, that improves your throughput, decreases length of stay, and improves workloads for hospitalists. Are you making your hospitalists pay the discharge tax?
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.