During a patient’s “journey” in the hospital, they may be seen by many different caregivers: Admitting, attending and subspecialty providers, just to name a few. This can be an overwhelming experience not only for the patient but for the hospital itself. Typically, registration does a good job of trying to keep up with all the moving parts throughout the patient’s stay. However, we are starting to see the hospital medicine team take control of this process and move from provider/attending-based assignments to a team method of patient assignments, or even a hybrid model of the two.
Let’s dive into the differences between provider/attending-based assignments and the team method of patient assignment and what might be a fit for your hospital.
Provider-Based Assignments
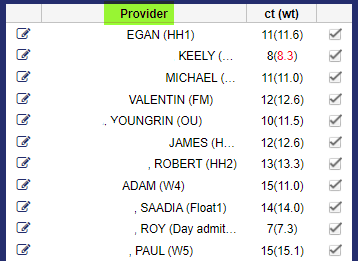
The traditional way of assigning patients to providers in a hospital setting is through provider-based assignments. In this scenario, patient assignments are dependent on which attendings are scheduled to work for that day. What we’ve increasingly seen is that hospitals then assign providers to a specific team for a given day, for a variety of reasons:
- This helps organize who is working where
- It can improve the hand-off or sign out process – you have a new provider taking over all that team’s patients, so they do one hand off instead of multiple hand offs
- It helps the list maker have some rules, whether using a patient assignment software like ours, Assign, or doing patient assignment manually. For example: some hospitals will have a float team. Now the list-maker knows that this provider is part of a float team and they can get anyone – easy to assign patients to any provider on a float team. Or perhaps it’s a geographic team – like “Team West 7.” These providers should only get patients on West 7.
However, in this model, since this type of team information is done at the scheduling level, you wouldn’t see this in the EHR.
Team Method of Patient Assignment
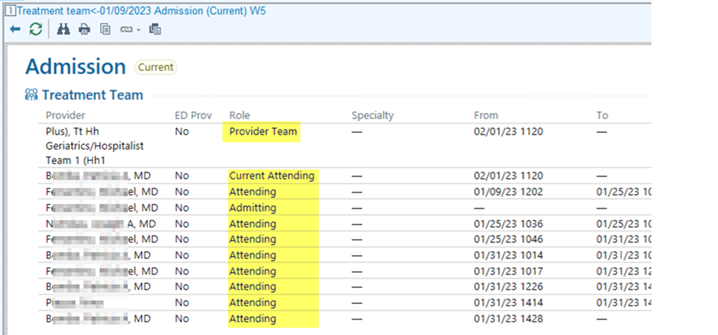
We’re seeing more and more of our clients opt for a team method of patient assignment. In this type of patient assignment model, a patient is assigned to a Care Team. The patient never changes teams; however, the individual care members on the team (attendings, NPs etc.) may change.
In the team method of patient assignment, you assign a patient to a team and then build the care team around it. Since the patient is always staying on the care team they were assigned to, this tends to be an easier way to get updates and communicate changes; such as:
- Easier for other groups in the hospital to communicate, look up provider information, and cover
- A nurse or case manager doesn’t need follow a specific doctor, they can follow a team instead
Patient Assignment Comparison: Provider-Based Assignments vs. Team Method of Patient Assignments
| Provider-Based Assignments | Team-Based Assignments | |
| How patients are assigned | Patients are assigned to a provider, dependent on whichever provider is scheduled that day. Typically, a provider is then assigned to a specific team for a given day. | Patients are assigned to a specific care team based on a clinical or organizational need (OBS, Geriatric team, Team Blue). Each team is made up of different roles: Attending, Nurse, NP, and Case Manager, for example. |
| What type of team-based assignments are involved? | This would be an example of team-based assignments at the schedule level. The “team” information is only available in the scheduling software. | This is an example of team-based assignments at the EHR-level. |
| Hand off/sign out process | When one provider’s shift ends, one new provider takes over all of that provider’s patients. Different providers may want to hand off to specific team members. | When one provider’s shift ends, a new provider replaces that role on the team. Hand-off information is shared within the team. |
| Who can see patient and provider assignments? | The provider’s teams are assigned at the scheduling-level so this information is only available in the scheduling software. | The teams are created at the EHR-level for everyone to see. That information can be sent downstream to anyone in the hospital who needs it. Anyone can look up a team to see who is caring for the patient. |
Which model fits your hospital? There’s also the option of a hybrid model between the two. You assign patients to providers/attendings; you send that information outbound to the EHR; and then you can also assign that patient to a team.
How We Can Help, For Provider-Based or the Team Method of Patient Assignment Models
No matter which method you choose, we can help you optimize and improve your patient assignment process – so providers can be scheduled quicker and more efficiently, patients can get seen faster, and all provider/patient information gets transmitted to whoever needs it.
We do this in two ways:
- Assign, our patient assignment software, automates the patient assignment process so instead of creating rounding lists manually, our system imports your census and provider schedule, runs our rules engine to optimize your list (perhaps you want geographic considerations, or continuity of care), and then finalizes the list, integrated back into your EHR.
- More than just the software, we take a consultative approach to the patient assignment process – or problem!
There are so many different hospital systems that impact the creation of your daily rounding list. Often these systems are disparate and unorganized. Perhaps you have a schedule workflow where providers are scheduled such as Qgenda or Amion. Then you have an attending workflow where patients are assigned to an attending based on certain criteria. And then perhaps you want to do a team concept as well or a hybrid model as described above.
Often times, all these systems and workflows were all implemented at different times, in silos. What ends up happening is the real impact of how each system impacts the other and how they need to work together is not truly considered until the problem is exacerbated.
So what can we do to help solve this problem?
The first step is to analyze your different systems and identify how they would ideally work together and the best way to improve it. For example, we can map schedule team data to provider data to treatment team data, to have them in sync and talking to each other. Our interfaces and flexible integrations make this possible – turning siloed systems into one unified, in sync source of truth.
This really improves your entire patient assignment workflow – from how providers are scheduled to how patients are seen by whom and when.
Through mapping and a customizable outbound interface, medaptus lets you create your assignments in our system while keeping all the data in sync in your EHR without human intervention, a true labor savings benefit.
For example, let’s say Dr. Jones is on Team 1 (Qgenda) and assigned to Team Blue in Epic. Our outbound interfaces means we do the patient assignment process and automatically update the patient and team information in your EHR, so it’s visible to whoever needs to see it.
The key benefits:
- Instead of taking 2-3 hours to create your daily rounding lists, it gets done in a few minutes
- That means that vital information on which patient is assigned to which provider, gets communicated downstream throughout a hospital, quicker
- That means nurses are not waiting for attending information to put in orders or start seeing patients
- It means providers and nurses know who to see and speak to right when their shift starts
- Ultimately, it improves patient care and keeps your providers happier, too
Want to see what an improved attending-based or team method of patient assignment might look like for you? Get a demo of Assign here.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.