Although EHRs were primarily designed to digitally store patient health information, it’s become more and more common for hospitals to use EHRs for other purposes too – such as charge capture.
Since EHRs weren’t built as charge capture solutions, there are ways to optimize your EHR to solve workflow challenges when it comes to streamlining, capturing, and billing charges.
In this article, we’re going to focus on what is charge capture in Epic and how we help bridge the workflow and process gaps of EHRs when it comes specifically to outpatient infusion coding and billing. Outpatient infusion billing is notoriously complex – which is why it’s common that an EHR can’t accurately bill for all your outpatient infusion services.
Using other solutions, like medaptus’ automated infusion coding solution, Charge Infusion, which directly integrates with EHRs like Epic, Cerner, Meditech and more, can enhance your existing EHR and fill the gaps so you never miss a charge and you recoup any revenue that’s being left on the table. Let’s cover:
- What is charge capture in Epic?
- The complexities of outpatient infusion billing
- Charge capture gaps in EHRs
What is Charge Capture in Epic?
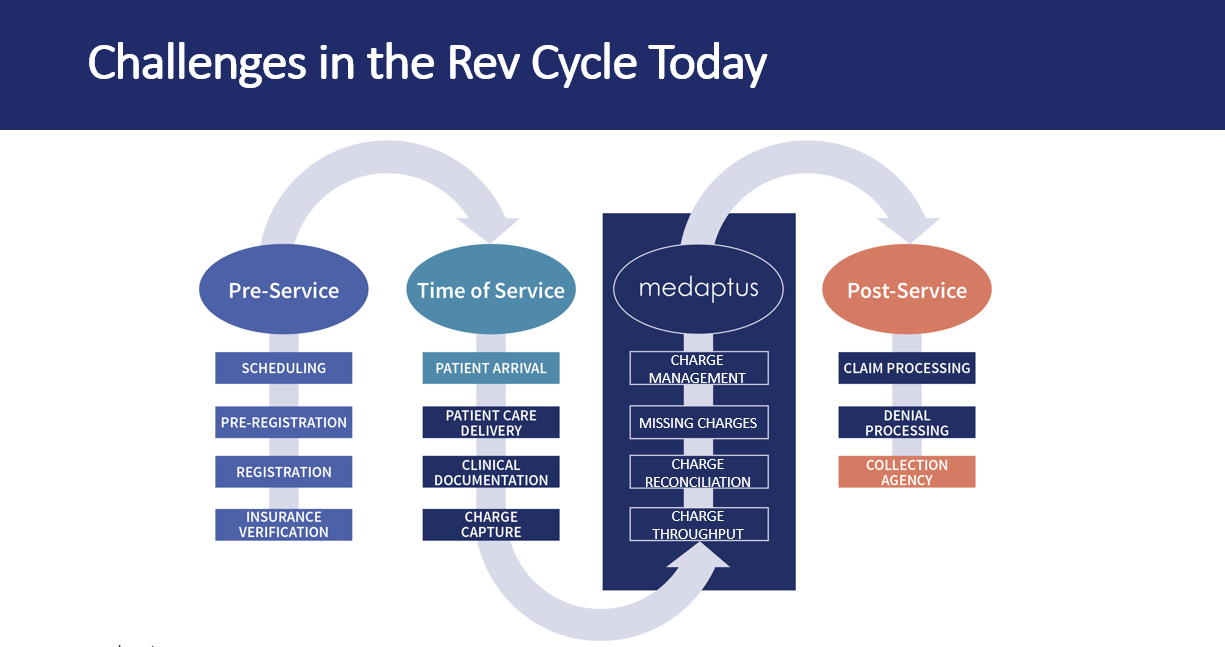
EHRs like Epic help do the job of capturing patient documentation, transmitting patient information to capturing charges and more. It’s an important solution that solves a lot of problems in the healthcare industry. But to optimize your workflows, there are solutions like ours that enhance what your EHR does and streamline other parts of the charge capture and revenue cycle process, specifically when it comes to outpatient infusion billing and coding.
In fact, when we audited various hospitals across the US, we found that up to 60% of rendered infusion services were unreported and unbilled for. In one facility alone, a major cancer center we worked with that delivers 130,000 infusions annually – they generated an additional $3.4 million a year by capturing previously unreported infusion revenue.
What are the gaps in your EHR that may be causing you not to capture or bill properly for all your outpatient infusion services? It comes down to two complexities.
Complexities of Outpatient Infusion Billing
Hospital departments that do high volumes of outpatient infusions, such as Emergency Departments and Oncology for example, need to bill for infusion services differently than inpatient infusions. There are two aspects to this:
- The duration of outpatient infusion – start and stop times
- The hierarchies of infusions
Duration (Start and Stop Times)
For outpatient infusions, infusion billing codes are determined by the duration of infusion. For every infusion, you have to document the start and stop times. Only then can you properly complete your infusion billing.
A short infusion is any infusion under 16 minutes while a prolonged infusion is 16 minutes or more and the payment rate is different for each type. The difference of one minute or even a second can have a significant impact on revenue. When a department is doing hundreds of infusions daily, inaccuracies for even a small percentage of infusions add up and can have a significant impact on hospital revenue.
In fact, one hospital we audited was automatically downgrading their infusion times if it was between 16 minutes and 1 second, to under 16 minutes. This caused them to be billing them as a “short” or “push” (when they were entitled to bill more!) which drastically impacted their revenue.
Infusion Hierarchies
Infusion hierarchies refers to how infusion services can be properly coded and billed to maximize the amount of revenue you get. Infusion coding must be done according to a specific hierarchy—for example, if you are giving multiple types to the same patient in the same period (like chemo and hydration for example), you would bill the chemo drugs before therapeutic drugs before hydration drugs—and the number of units of each is directly determined by the duration of the infusion itself. Unlike most medical procedures and services, infusion coding is actually more like a mathematical equation.
EHRs weren’t built to calculate these complex outpatient infusion charge scenarios. Using another system, like our Charge Infusion product, helps you bridge this gap with your EHR.
Charge Capture Gaps in EHRs
While EHRs like Epic can help with some aspects of charge capture, there are a few gaps that would cause challenges in your workflow. This is especially true for outpatient infusion coding and billing. Since EHRs are an integral part of the process, you can easily integrate solutions like ours to ensure that no data is lost and you’re still operating out of the EHR. For example, one of the Massachusetts-based hospitals we work with integrates our automated infusion coding and billing solution, Charge Infusion, directly into Epic. We get their infusion data from Epic, we run them through medaptus’ proprietary rules algorithm, taking into account the duration and hierarchy complexities, and then send the data back into Epic to be billed out. One tool, one easy integration, one complete solution – for maximum infusion revenue.
Here are a few other charge capture gaps in today’s EHRs:
- Charge Management – Missing Charges
While you can submit charges, EHRs don’t analyze any charges – there is no “charge management” feature that helps you identify if there are any missing charges. Instead, you have to do this manually.
Another aspect of this is the manual work that coders have to do to review every single charge. If there is missing documentation, or encounters that were billed incorrectly, they either have to chase the provider to get more information or change the billing code, and under-code. This causes a lot of lost revenue.
- Documentation – Is the right documentation attached to the charge?
Let’s say a provider submits a charge in the EHR with their documentation, the coder reviews it, and the documentation doesn’t match what they should’ve charged for. That deficiency needs to be communicated back to the provider. You cannot bill out that level of that code because it doesn’t match the documentation, or the coder would need to down-code the code. Those situations occur all the time.
Perhaps you need documentation on how that encounter relates to that charge, or maybe the charge was submitted without a diagnosis code. Then, there are situations where you are not able to bill the entire encounter out, let alone just have it down-coded. The result is a full loss of a charge.
- Coding – Too much manual work
When it comes to coding, EHRs don’t automatically help you understand things like if the right diagnosis code is listed. The coding team has to review and analyze charges – and this is all done outside Epic, too. They have to communicate with providers to get any additional information or correct charges that are missing information.
With medaptus, you get a complete view of every charge and their status and know exactly what information is required to get this to billing.
Final Notes
EHRs are necessary and vital tools for every hospital – but were never intended to be a complete solution to the entire revenue cycle process. In this article, we showed you why outpatient infusion billing is complex and needs to be handled separately in order to maximize your revenue and ensure you are not underbilling for services you rendered. We also talked about the charge management and documentation gaps that can exist and how to solve them.
By resolving these costly workflow issues, you can ensure your revenue cycle process is operating smoothly – and that you are recouping every dollar that’s on the table.
Want to learn more? Check out our new video series on outpatient infusion coding and billing here.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.