With the increasing volumes of patients that hospitals are seeing daily, do you wonder if patients are being distributed equally? Do you wonder if your hospitalists are seeing more patients than they can handle?
Well…
For operations or hospital leadership, the faster you can discharge a patient = more profit for the hospital. For hospitalists, efficiently discharging patients means length of stay (LOS) decreases. Unnecessary days in the hospital may lead to increased hospital-acquired patient complications (e.g., healthcare-associated infections, falls) and increased costs for patients and healthcare systems. The average length of stay (LOS) for a hospitalization is 5½ days.
The National Library of Medicine conducted a study by hospitalists at Tufts-New England Medical Center in Boston, MA. The study consisted of two groups: one with a hospitalist group and one without. The hospitalist group reduced LOS from 3.45 days to 2.19 days. Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists expeditiously discharging patients.
Even though leadership encourages timely discharges, physicians are rarely incentivized to do so, since once a physician discharges one patient, they get assigned a new patient – which is often more work than rounding on a current patient. Patient assignments end up being a revolving door for the physician – a 1 in 1 out model.
Let’s look at this in Scenario 1 that happens in your hospital today:
Dr. Bob – Discharges 5 patients today, gets 5 new patients tomorrow:
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 Discharged | New Patient – More work |
| Patient 12 | Patient 12 Discharged | New Patient – More work |
| Patient 13 | Patient 13 Discharged | New Patient – More work |
| Patient 14 | Patient 14 Discharged | New Patient – More work |
| Patient 15 | Patient 15 Discharged | New Patient – More work |
| Total Headcount: 15 |
Dr. Jeremy, AKA “The Lazy Discharger”
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 | Patient 11 |
| Patient 12 | Patient 12 | Patient 12 |
| Patient 13 | Patient 13 | Patient 13 |
| Patient 14 | Patient 14 | Patient 14 |
| Patient 15 | Patient 15 Discharged | New Patient – More work |
| Total Headcount: 15 |
Dr. Bob just got taxed! He discharged patients more effectively than Dr. Jeremy but was essentially penalized the next day by getting five new patients. This model is often used because it’s easiest to maintain, and everyone gets the same headcount each day.
The discharge tax is a term used to describe when a provider discharges a lot of patients, they will get assigned new patients tomorrow that will bring your workload right back up.
What if you could ease the burden of the discharge tax?
Using Assign, our automated patient assignment solution, you can remove the burden of the discharge tax by weighing new patients as 1.5 (aka a patient and a half = more work) so that hospitalists that discharge don’t automatically get the exact same number of new patients.
Scenario 2: Weighing “New Patients” as 1.5
Dr. Bob
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 Discharged | New Patient – 1.5 |
| Patient 12 | Patient 12 Discharged | New Patient – 1.5 |
| Patient 13 | Patient 13 Discharged | New Patient – 1.5 |
| Patient 14 | Patient 14 Discharged | |
| Patient 15 | Patient 15 Discharged | |
| Total Workload of 14.5 |
Dr. Jeremy
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 | Patient 11 |
| Patient 12 | Patient 12 | Patient 12 |
| Patient 13 | Patient 13 | Patient 13 |
| Patient 14 | Patient 14 | Patient 14 |
| Patient 15 | Patient 15 Discharged | New Patient – 1.5 |
| Total Workload – 15.5 |
We are still maintaining workload balancing but Dr. Bob is not penalized as hard – he gets two less patients than in scenario one.
I’ve been recently working with Good Samaritan Hospital and one thing that was very important to them was decreasing LOS and balancing patient assignments. We were able to solve these problems by evenly balancing all new patients and ignoring workload balancing and headcount.
Scenario 3: Six available new patients amongst two providers – Evenly balanced amount all team members.
Dr. Bob
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 Discharged | New Patient – More work |
| Patient 12 | Patient 12 Discharged | New Patient – More work |
| Patient 13 | Patient 13 Discharged | New Patient – More work |
| Patient 14 | Patient 14 Discharged | |
| Patient 15 | Patient 15 Discharged | |
| Total Headcount: 13 |
Dr. Jeremy
| Day 1 – Beginning of Morning Shift | Day 1 – End of Shift | Day 2 – Beginning of Morning Shift |
| Patient 1 | Patient 1 | Patient 1 |
| Patient 2 | Patient 2 | Patient 2 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 3 | Patient 3 | Patient 3 |
| Patient 4 | Patient 4 | Patient 4 |
| Patient 5 | Patient 5 | Patient 5 |
| Patient 6 | Patient 6 | Patient 6 |
| Patient 7 | Patient 7 | Patient 7 |
| Patient 8 | Patient 8 | Patient 8 |
| Patient 9 | Patient 9 | Patient 9 |
| Patient 10 | Patient 10 | Patient 10 |
| Patient 11 | Patient 11 | Patient 11 |
| Patient 12 | Patient 12 | Patient 12 |
| Patient 13 | Patient 13 | Patient 13 |
| Patient 14 | Patient 14 | Patient 14 |
| Patient 15 | Patient 15 Discharged | New Patient – More work |
| New Patient – More work | ||
| New Patient – More work | ||
| Total Headcount: 17 |
Dr. Jeremy and Dr. Bob each get the exact same number of new patients each morning – three and three. In this model, we are rewarding providers for discharging, and penalizing providers for not discharging.
Good Samaritan– Evenly Balance of New Patient – How we did it
With their goals in mind, we set up a custom rule for Good Samaritan in Assign to help evenly distribute patients so that no providers were penalized, and workloads were balanced. In Assign, we did the following:
We had to accurately identify a “New Patient” if they were admitted between certain times.
In the old model, we used admission time if a patient was admitted between X:00 AM – X:00 PM. This was not always accurate for many reasons.
New logic:
Was the patient assigned yesterday? If the answer is no, then they are a new patient. This captures all scenarios of new patients to the Hospital Medicine team.
Next, we created a new rule on Assignment Workflow Table: Balance Evenly NewPatient
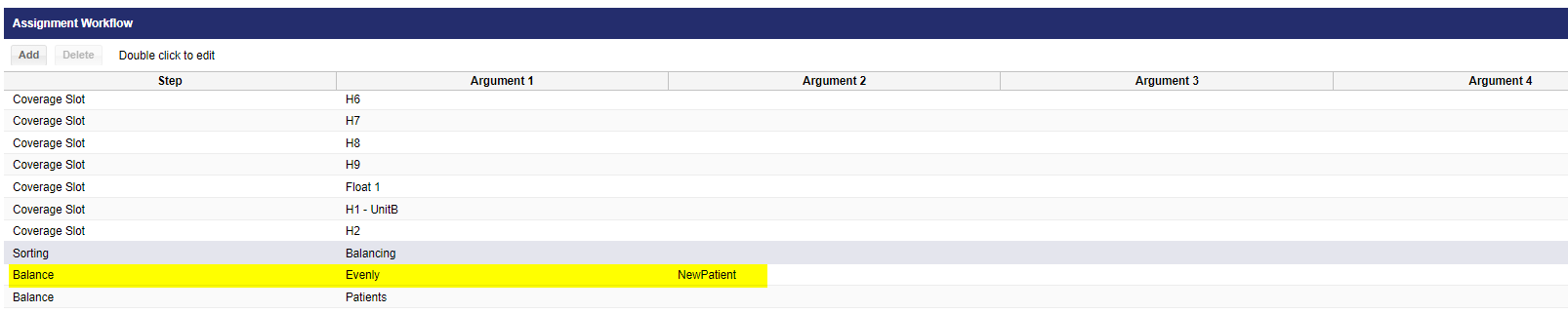
Lastly, we used “N/A” instead of “calculate” for the provider’s MAX.
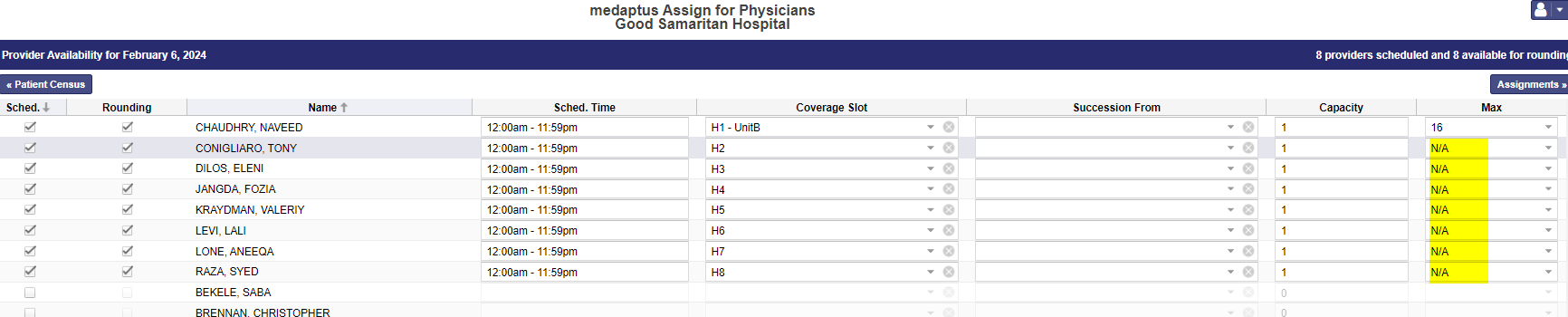
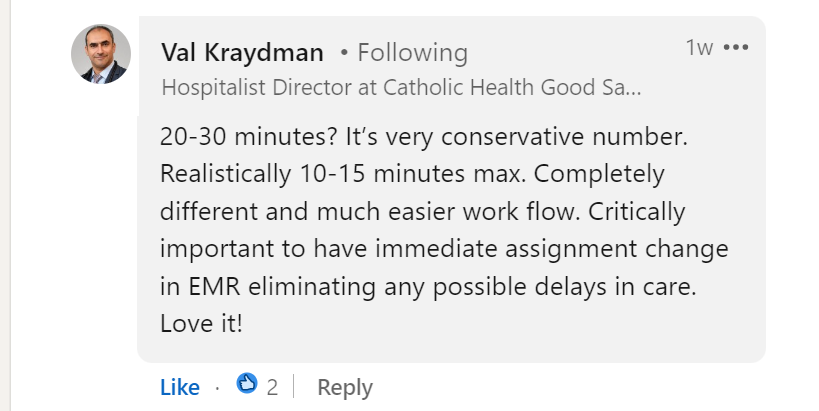
As you can see, the discharge tax can be a burden on many different roles in any organization and can have a ripple effect. Not only was Good Samaritan suffering from the discharge tax, but they were also struggling with heavy and unfair workloads. Prior to medaptus, their patient assignment process was being done the manual way which was becoming time consuming and complicated. Now, Good Samaritan is experiencing greater provider satisfaction and a fully automated fair patient assignment solution that can be done efficiently in 15-20 minutes.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.