As a physician, you may be wondering how to track some key performance measures or want to see a simple dashboard of your charges in real-time. Or, if you are a busy executive in charge of a physician group, it is also equally important to have real-time dashboards so you can keep a pulse on how your organization is performing.
At our medaptus Academy last year, Jaclyn Corbett, Product and Release Manager at Medaptus, gave a session focused on physicians and how they can use Charge Pro to measure performance, charges in the billing process, evaluation, and management (E&M), readmission rates, and missing charges.
The next five reports will help you stay organized by getting a good sense of how your billing processes are working and how you are operating.
Charge Summary Report
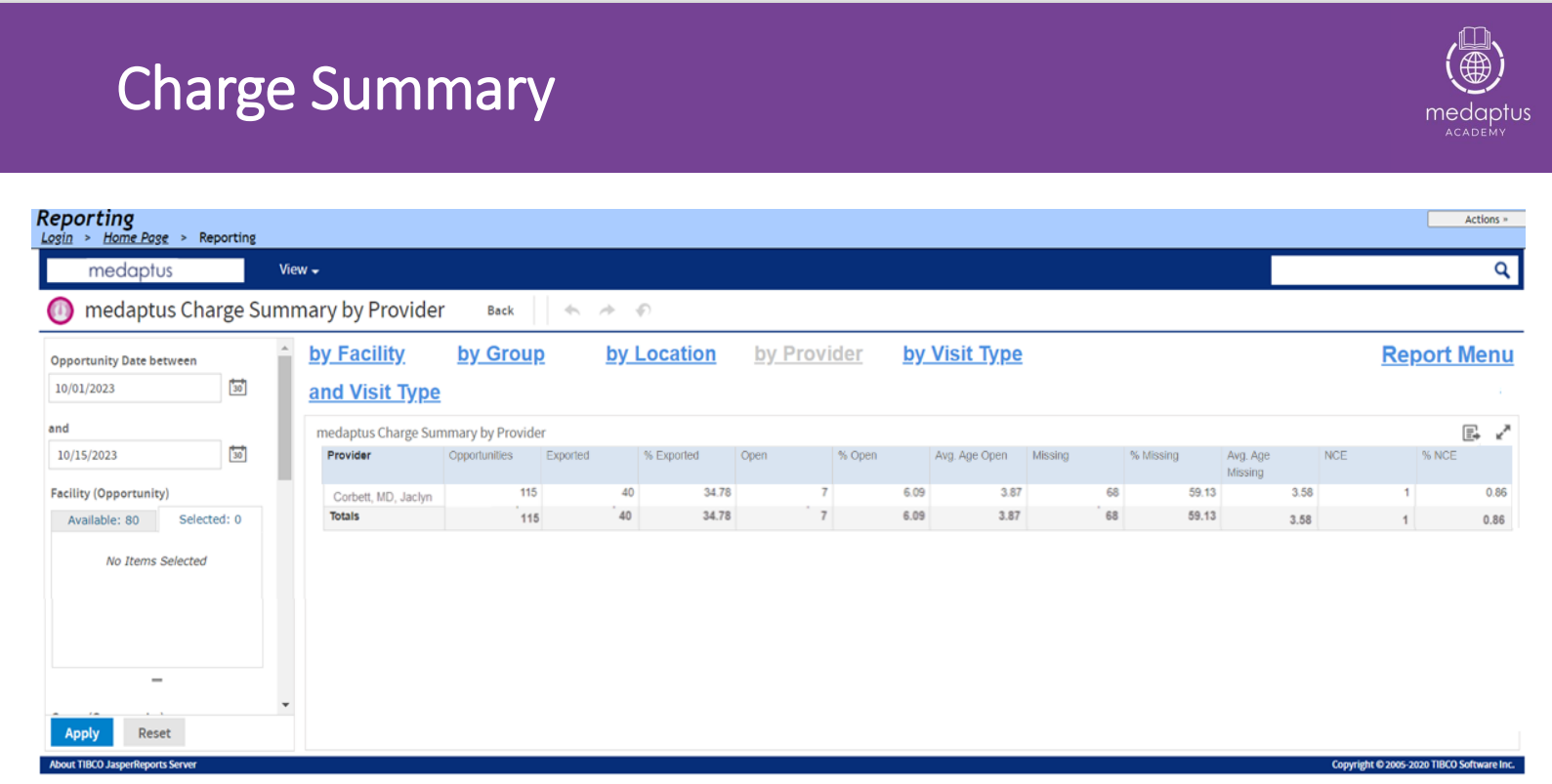
This is a report for individual providers. This gives you an idea of how your charging is going for a specified among of time you have selected. This is great if you are a Chief Medical Officer, and you need to see how your providers in the organization are in terms of their charges and where they are in the process.
Here is an example of filtering by provider. You could run this report by group as well if you wanted to see the numbers at a glance.
As the name implies, you can see where a physician’s charges are in the billing process. Here you can see exported charges, average number of charges in open status, missing charges (this provider has not billed for 68 of these opportunities) and average number of days the charge has been in an open status.
Provider Productivity (RVUs) Report
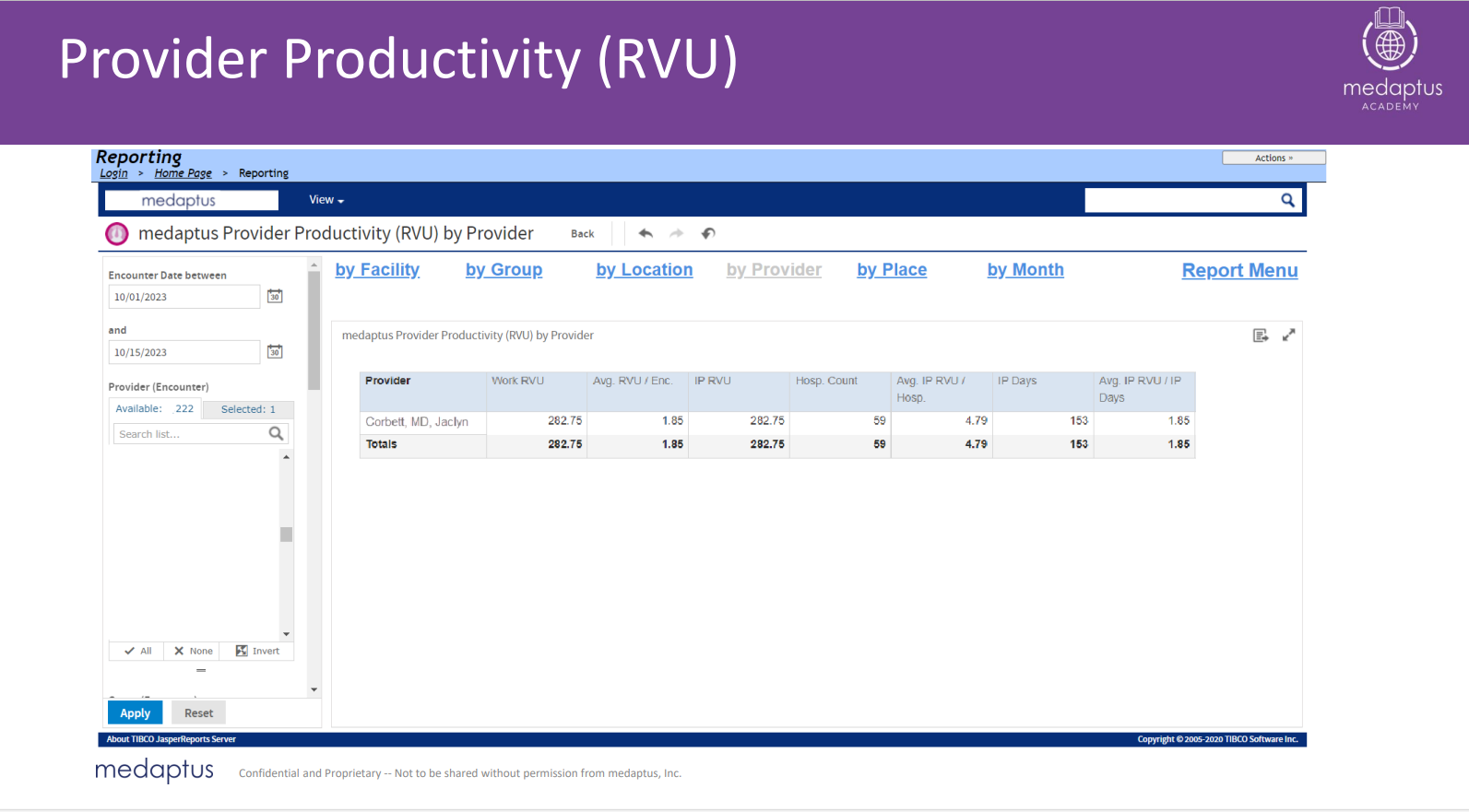
This report will show you, based on the time you select, how many work RVUs you have based on the CPT codes you have billed. You can see working RVUs and average RVUs per encounter. This can be broken up by inpatient and outpatient RVUs as well. This report is helpful and important to keep track of where providers are because there is a direct correlation between RVUs and their pay, or a bonus they are receiving.
Missing Charge Report
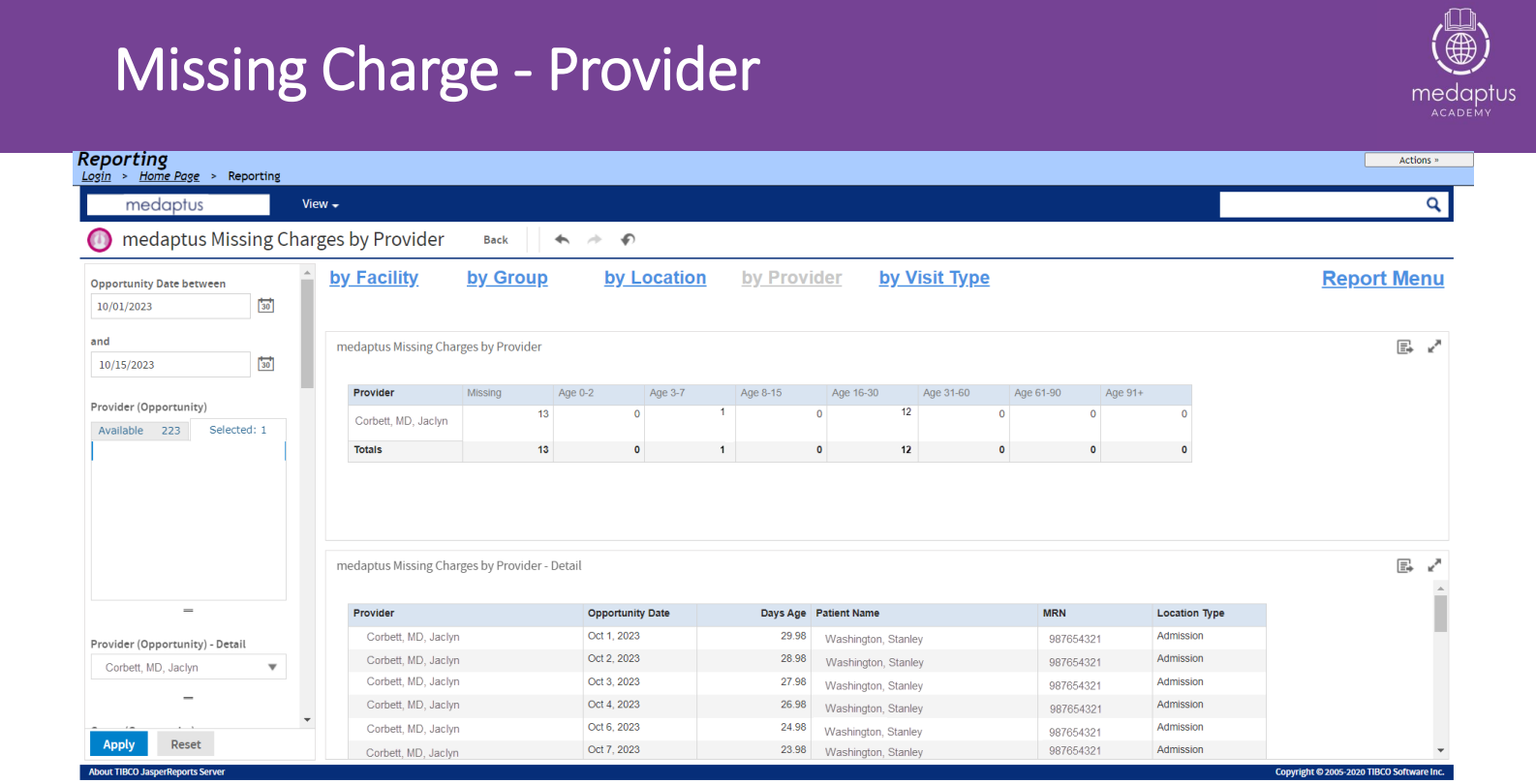
In the other reports, you might have noticed a column indicating you have missing charges. You may be wondering, “where are these missing charges? What patient am I missing charges on?” By running this report by provider at the top and selecting a provider in the “Provider Opportunity – Detail” box on the bottom left side, you will then be able to see the specific patients and dates you are missing charges for. Below you can see there are 13 missing charges and ages of the charges that are missing. For example, there are 12 charges that are 16-30 days old, and these are the ones you want to pay attention to, so that you avoid missing filing deadlines and missed revenue.
E&M Distribution Report
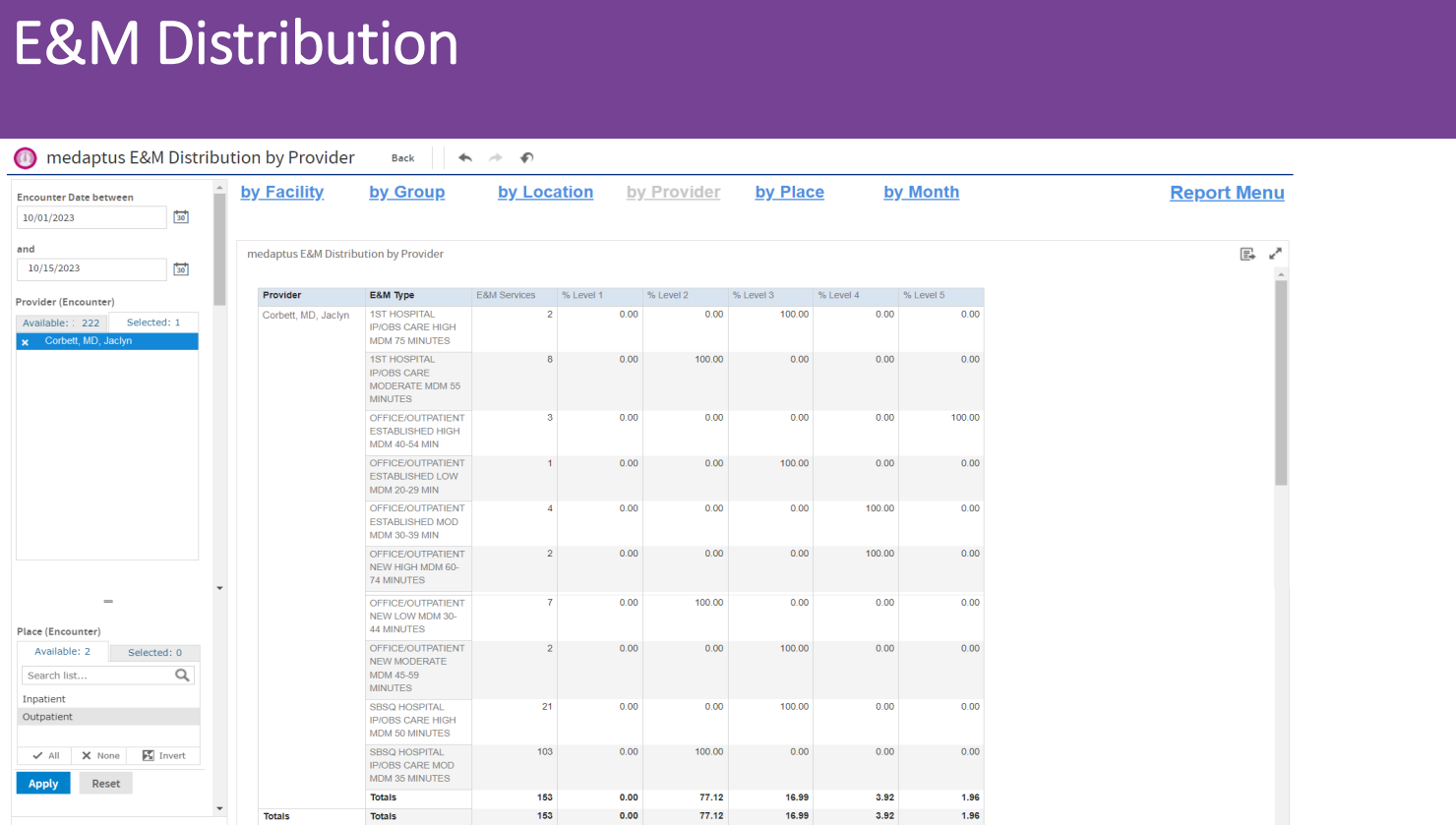
There are no fixed rules on E&M distribution reports. It can vary based on the specialty of the provider or the nature of your practice. A few things to look for in this report to keep you on track:
- You want your lower-level codes to be lower in the amount you billed
- You want most of your codes to be in the average range
- You want your higher-end codes to be a little lower
Imagine a bell curve. Too many codes in one area could lead to audits, or it could mean inadequate care. Too many level 4s and 5s could mean a provider is billing unjustifiably high and could lead to audits.
Readmission Rate Report
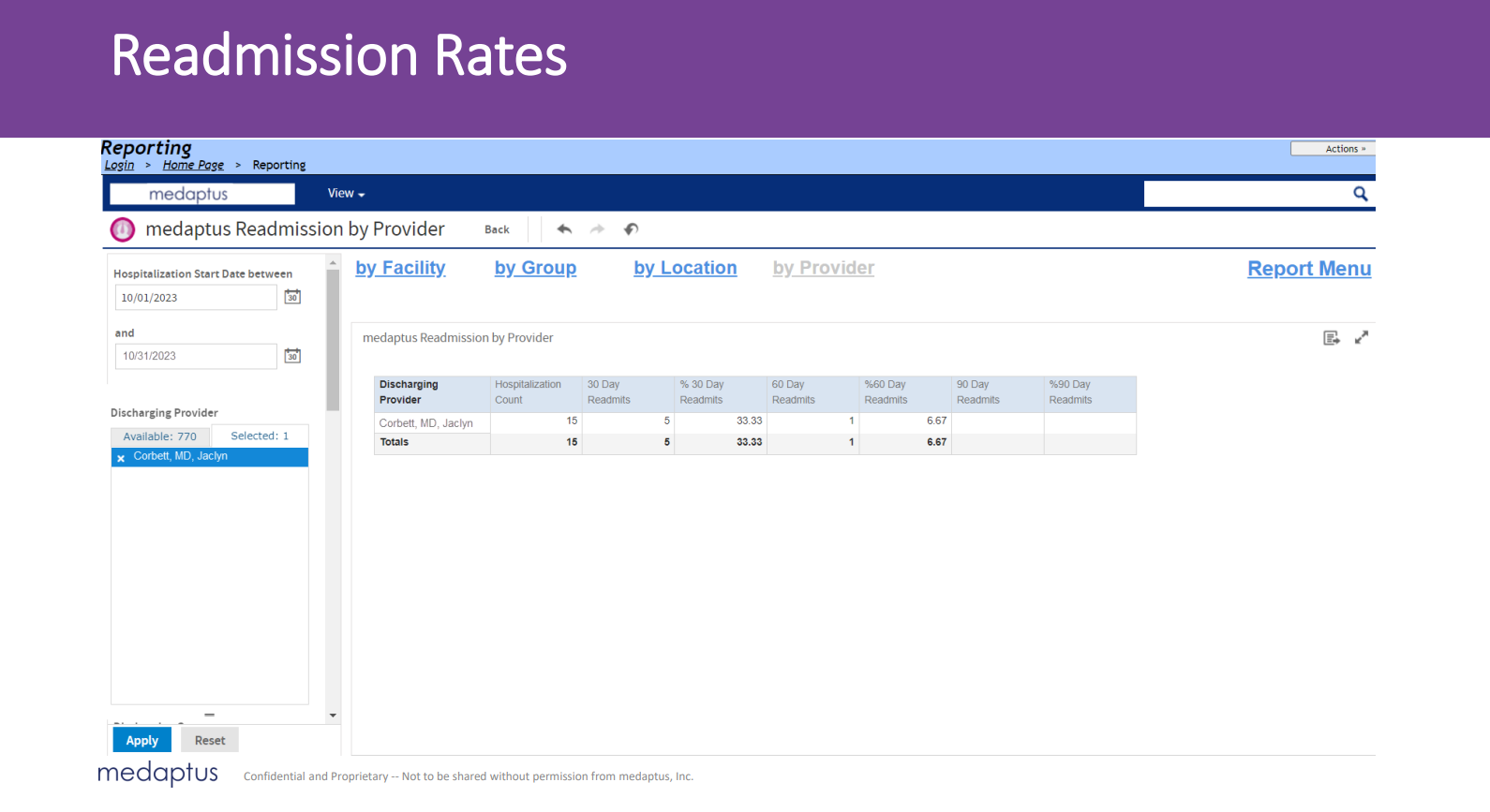
Readmission rates are often key performance indicators in an organization for physicians.
From this report, Dr. Jaclyn had 15 patients readmitted: five readmits within 30 days, one within 60 days, and the other nine were outside of the 90 day range.
To know if you are performing well in this category, it would depend on your organization’s acceptable readmission rates, then you would use this report to determine if your readmission rates are in line with those readmission goals.
Could these reports help your providers?
This is just a high-level overview of some reports within Charge Pro that can help you improve your billing, readmission, and productivity as a physician. As a Chief Medical Officer, or someone who oversees physician billing and documentation, these quick and easy-to-use reports allow visibility into the performance of each provider immediately for your convenience.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.




