It’s time to talk about continuity of care. In hospital medicine, one of the biggest areas of concern is maintaining continuity of care with our patients. It’s already disturbing to patients to come to the hospital and not be seen by their PCP (although given that it’s been more than 20 years since hospitalist medicine has been a reality, I imagine we’re seeing fewer and fewer people who are surprised by this), and often we make it worse for patients by having a rotating staff of docs who see the patient. How can we measure how well we’re doing with continuity of care?
Some discontinuity, or course, is unavoidable. None of us work 24 hours a day, 365 days a year. So, there are always going to be handoffs. Unfortunately, sometimes we can have more than we would like. For example, you could have a patient admitted Thursday night by the nocturnist, rounded on Friday by the regular weekday doc, then have a new doc for Sat and Sun, and then have a new doc to beginning the week on Monday. So, over the course of 5 days in the hospital, the patient has had a total of 4 doctors – and that’s not counting the nighttime hospitalist for issues in the middle of the night, or all of the specialists who may be involved. Clearly we want to better than this, but how can we measure this so that we can see if our quality improvement projects are actually helping
The simplest measure is just a raw count of the numbers of doctors from the hospitalist group that are involved with the patient. So you simply count up all of the doctors who submit a charge for the patients and you get your number. This could be as low as 1, but is more likely to be at least 2, and depending on LOS (length of stay), could be a lot higher. In fact, that leads to the next possible refinement where you divide the number of docs by the LOS. So if you have 2 docs and a 7 day LOS, you have 2/7 (0.29) docs/day. Obviously, the lower this number is, the better the continuity of care is. A 7-day LOS with only 1 doc would give you 1/7 (0.15) docs/day (and this probably about the lowest you’ll see for any given patient). A 5-day LOS with 4 docs (as in the example above) would give you 4/5 (0.8).
Now if you want to go a little deeper, there’s another measure you can use which is probably a better metric for looking at continuity of care the takes into account the realities of hospitalist medicine. When you look at any given patient, there is going to be one doctor who sees that patient the most times. This would be considered the “primary hospitalist”. We can then look at what percentage of visits to the patient were done by the primary hospitalist. If you have a 4-day LOS with 4 visits:
- H&P (doc #1)
- 2 daily visits and a discharge (doc #2)
Then doc #2 is the primary hospitalist, and 3/4 or 75% of the visits are by her.
A different patient (say the weekend patient described above) could have:
- H&P Thursday night (doc #1)
- Daily visit Friday (doc #2)
- Daily visits Sat and Sun (doc #3)
- Discharge Monday (doc #4)
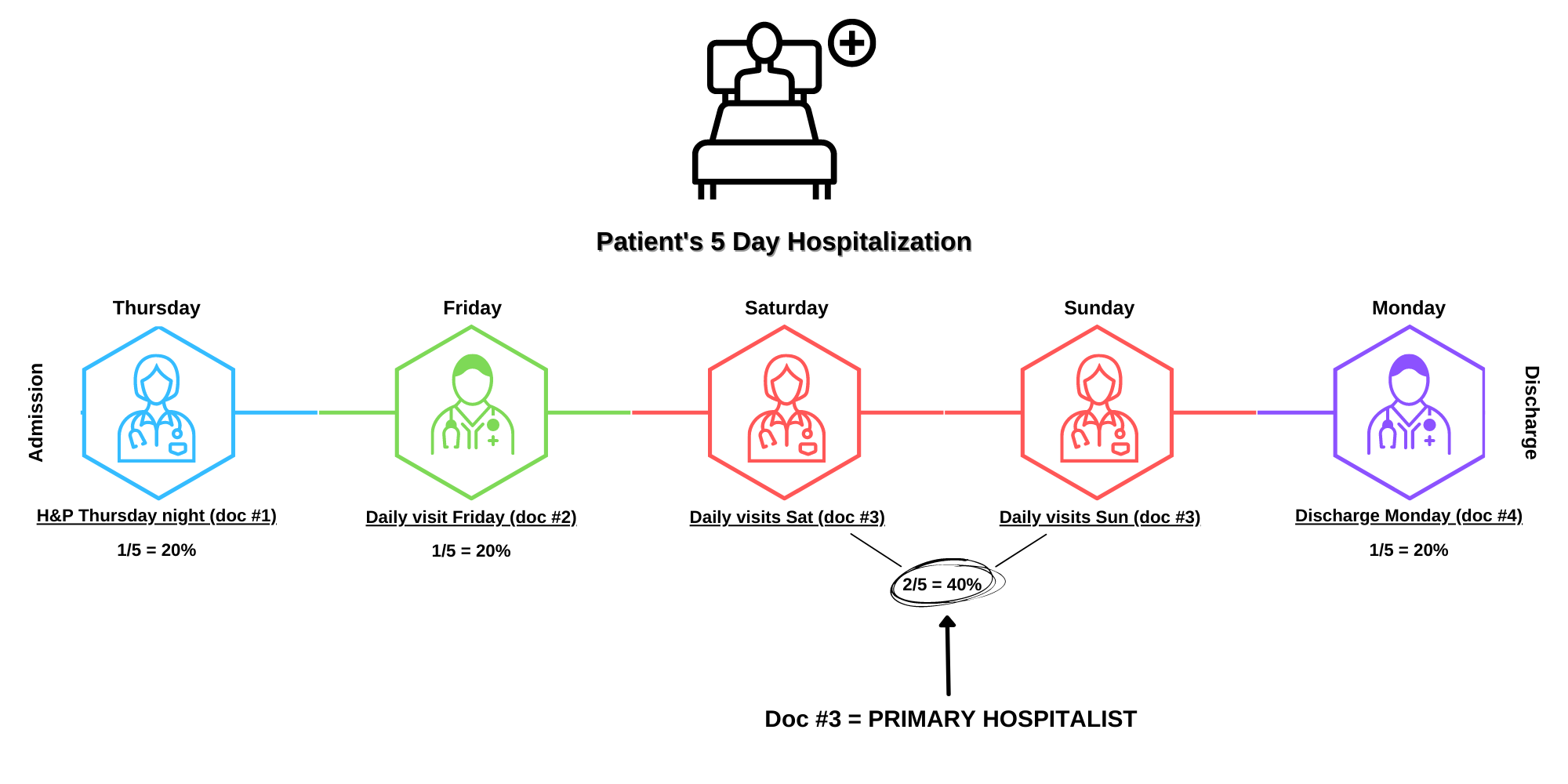 Now, Doc #3 is your primary hospitalist (since she has the most visits), and 2/5 or 40% of the visits were done by her. You could try to get fancy and start weighting different types of visits differently, but I don’t think there’s much benefit to it. This metric, as is, gives you an excellent sense of how much discontinuity there is. It allows you to track over time how your practice is doing with having most of the visits performed by the primary hospitalist. If you change your work models (e.g. eliminate dedicated daytime admitters and increase your rounders), you could then easily see the changes in your continuity. You could even then begin to track how your patient satisfaction scores correlate with changes in continuity, but that’s a story for another time.
Now, Doc #3 is your primary hospitalist (since she has the most visits), and 2/5 or 40% of the visits were done by her. You could try to get fancy and start weighting different types of visits differently, but I don’t think there’s much benefit to it. This metric, as is, gives you an excellent sense of how much discontinuity there is. It allows you to track over time how your practice is doing with having most of the visits performed by the primary hospitalist. If you change your work models (e.g. eliminate dedicated daytime admitters and increase your rounders), you could then easily see the changes in your continuity. You could even then begin to track how your patient satisfaction scores correlate with changes in continuity, but that’s a story for another time.
Read Part 1 of the Hospitalist Metrics Blog Series: Measuring Length of Stay for Hospitalists
Read Part 2 of the Hospitalist Metrics Blog Series: E/M Distribution
References: https://codingintel.com/em-frequency-data-for-hospitalists/
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.





