Charge Capture Essentials
For anyone new to revenue cycle management in healthcare, the term ‘charge capture’ may be unfamiliar. It may even sound like something you would do to improve the battery life of a phone. But in the world of healthcare, it is really the process of recording and submitting provider billable services for reimbursement from a payer.
On the surface it seems simple enough: a provider documents the service provided (the procedure) and the reason why (patient diagnosis). This is the basic process for any service transaction. But in the medical arena uniquely, there is much more complexity governing the process.
With the advent of mobile computing just over 20 years ago, savvy entrepreneurs and doctor technologists hypothesized that personal digital assistants could greatly reduce the healthcare system’s
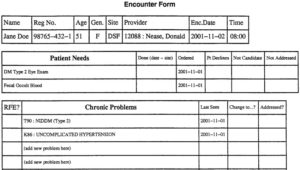
Encounter Form Example.
dependency on paper. Suddenly doctors were dictating notes on their phones and sending prescriptions electronically while walking.
Charge capture was one of the earliest applications to deploy on a mobile device. Previously the encounter form was the core mechanism by which a doctor billed for his or her services. This document typically indicated the physician’s charge, represented by circled codes on a photocopied form. Until electronic health records became widespread in nature, this was the manual process most provider groups undertook despite the risk of lost paper and lack of portability.
Even today, with the majority of doctors sitting at a workstation during a visit or using a smartphone, there are still challenges that seem easily most addressed by paper. For example, the provider that rounds at a small rural hospital with lack of EHR access or the doctor rounding at a community nursing home.
Unfortunately, a paper based process cannot fully reflect all of the requirements that charge capture entails. And at the end of the day it is the physician that is legally liable for accurate, compliant charge capture – not the individual hired to perform data entry. There is tremendous scrutiny of physician charges to ensure overpayment does not occur. Should an audit reveal a pattern of overcharging, there are significant financial and legal ramifications.

Ensuring Compliance
At the heart charge capture are ‘the codes,’ thousands of numeric procedure and diagnosis codes that can change annually with new codes introduced and others retired. Use an expired code – or the wrong code – and those are causes for denial. Then there are the rules, a countless number of rules that fall under an alphabet soup of categories (i.e., CCI, NCD, LCD) that are dependent on a variety of factors including payer type, geographic location, and provider specialty. If a submitted charge violates just one rule, the provider or institution will not receive payment until the error is corrected and the claim is re-submitted. The process of working a denial is time consuming and resource intensive. For some practices it just is not worth the effort if a relatively low dollar amount is at stake.
Given the potential compliance and revenue risk associated with charge capture activities, most groups employ a team of individuals to manage and monitor the process with or without the aid of information technology. Members of the revenue cycle team typically spend a great deal of time reconciling visits or rounding lists to avoid missing charges and reviewing submitted charges for accuracy. Without automation, the process can be very tedious and time-consuming and also requires specialized training and management oversight.
Electronic Charge Capture Emerges
Knowing that it is vital for billing to happen in a timely manner many groups use a charge capture software application to streamline the process with embedded compliance support. For some groups this is a web-based solution that is interoperable with their EHR. For other groups the sort of mobile charge capture technology described earlier in this piece is still used today to document thepatient encounter at the point-of-care or on the move. In either case, those organizations that leverage information technology to support their charge capture activities realize significant benefits in revenue optimization, physician satisfaction, compliance, and staff productivity.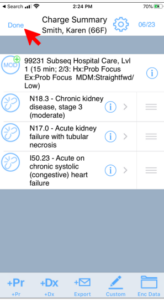
To keep reading about the evolution of charge capture technology, check out the rest of the posts in this series:
- What is Charge Capture? Part II: Stakeholder Expectations of Electronic Charge Capture
- What is Charge Capture? Part III: Tools for the Back Office
- What is Charge Capture? Part IV: Charge Capture KPIs and Actionable Insights
- medaptus Expands Charge Pro Solution with Launch of Consult and Documentation Modules
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.





